CPR certification provides essential skills for responding to medical emergencies. In Sacramento, numerous organizations offer training, equipping individuals with the knowledge and practical ability to administer cardiopulmonary resuscitation. This guide outlines options for obtaining CPR certification in the city, aiming to demystify the process and highlight key considerations.
To navigate the landscape of CPR certification in Sacramento, understanding the types of courses available is crucial. The American Heart Association (AHA) and the American Red Cross are the two primary national organizations that set the standards for CPR training. Many local providers in Sacramento are authorized by these bodies to conduct courses. Therefore, when searching for a certification, it’s important to recognize that you’ll likely be completing a program accredited by one of these established institutions.
CPR certification isn’t a one-size-fits-all proposition. The specific requirements and the type of certification you need depend largely on your intended use of the skills. Are you seeking certification for personal enrichment, or is it a professional mandate? This fundamental question will guide your search.
Professional vs. Lay Rescuer Certification
Professional Rescuer Certification
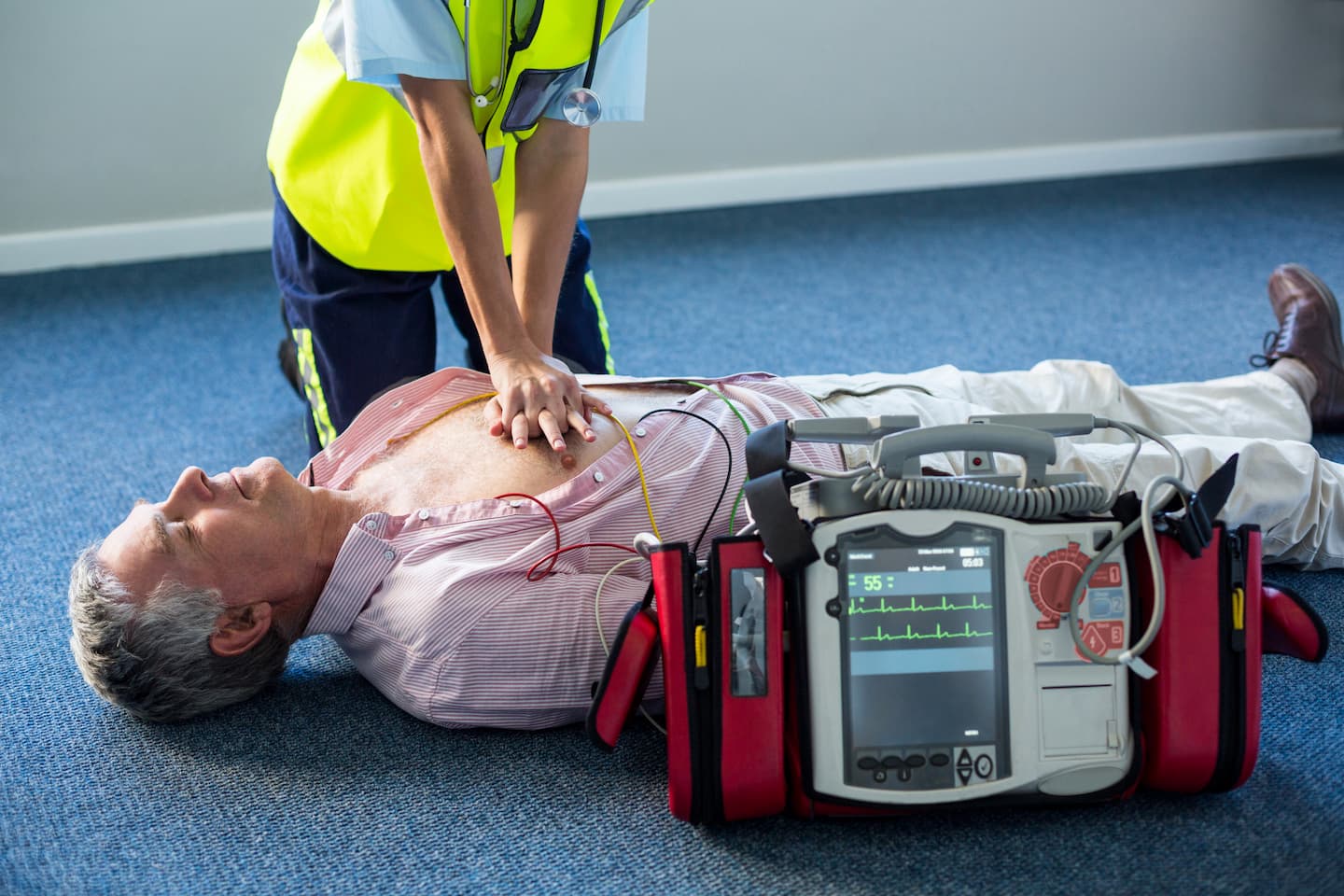
This level of certification is typically required for individuals in healthcare professions or those who may be the first to respond to an emergency in a professional capacity. Think of nurses, doctors, EMTs, lifeguards, and daycare providers. These courses are often more in-depth, covering a wider range of scenarios and skills, including the use of advanced equipment. The rigorous nature of these programs ensures that professionals are well-prepared to handle a variety of medical crises.
American Heart Association (AHA) BLS for Healthcare Providers
The AHA’s Basic Life Support (BLS) for Healthcare Providers course is a widely recognized certification for those working in healthcare settings. This course emphasizes the importance of early recognition of cardiac arrest, prompt CPR, the use of an AED, and the management of choking. It covers one- and two-rescuer CPR for adults, children, and infants, as well as basic airway management and the use of a bag-valve-mask. The training focuses on the critical chain of survival: recognizing the emergency, calling for help, starting CPR, defibrillation, and advanced care. The BLS certification is typically valid for two years.
American Red Cross Basic Life Support (BLS)
Similar to the AHA, the American Red Cross also offers a BLS certification tailored for healthcare professionals. This program also adheres to the guidelines set forth by national resuscitation councils. It prepares individuals to respond to breathing and cardiac emergencies in a variety of pre-hospital and in-hospital settings. The curriculum includes recognition of life-threatening emergencies, how to give chest compressions, rescue breaths, and how to use an automated external defibrillator (AED) for adult, child, and infant victims. Like AHA BLS, this certification is generally valid for two years.
Lay Rescuer Certification
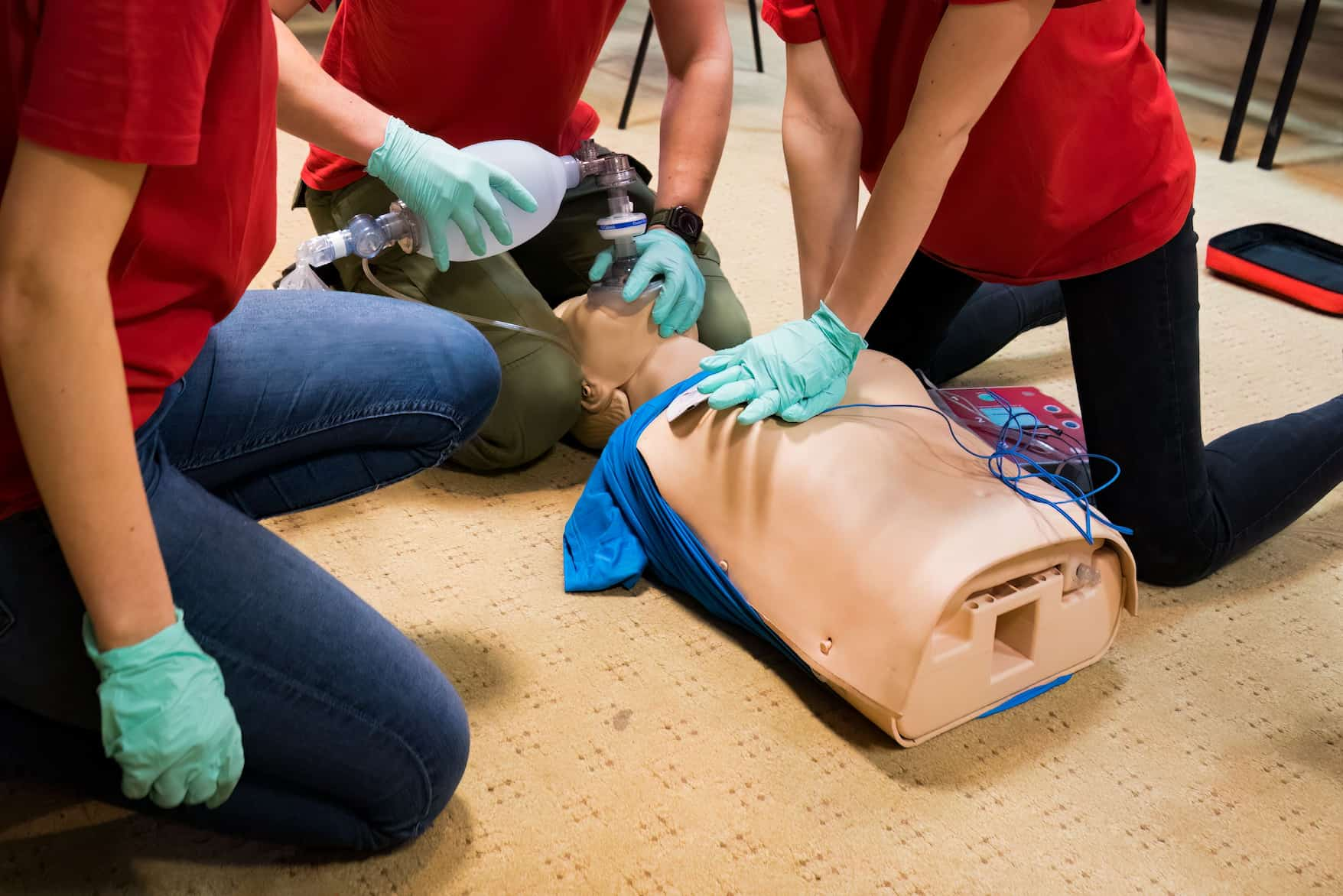
Lay rescuer certifications are for individuals who do not work in a healthcare setting but wish to be prepared to help in an emergency. This could include parents, teachers, coaches, community members, or anyone interested in acquiring life-saving skills. These courses, while comprehensive, are designed for a broader audience and may not delve into the advanced medical nuances required for healthcare professionals. They focus on the fundamental steps of CPR.
American Heart Association Heartsaver® CPR/AED
The AHA’s Heartsaver® CPR/AED course is designed for individuals who have little or no medical training but are required by their job or for other reasons to have CPR and AED certification. This course focuses on adult, child, and infant CPR and AED use. It provides participants with the knowledge and skills needed to respond to cardiac arrest and choking emergencies in the first few minutes until professional help arrives. The course often includes a hands-on skills testing component to ensure competency. The Heartsaver® certification is also typically valid for two years.
American Red Cross CPR/AED/First Aid
The American Red Cross offers a combined CPR, AED, and First Aid course that is highly beneficial for lay rescuers. This comprehensive program equips individuals with the skills to respond to a variety of emergencies, including sudden cardiac arrest, choking, severe bleeding, burns, and more. The CPR and AED portion covers adult, child, and infant victims. By combining these skills, individuals are better prepared to provide immediate assistance in a wide range of scenarios. This certification also generally has a two-year validity period.
Choosing a Training Provider in Sacramento
Sacramento boasts a diverse array of organizations that provide CPR certification. Your choice of provider can influence the course format, schedule, cost, and ultimately, the certification you receive. It’s akin to selecting a craftsman; you want someone skilled, reliable, and whose methods align with your needs.
Factors to Consider When Selecting a Provider
When making your selection, several key factors should guide your decision. These are the compass points that will lead you to the right training center.
Accreditation and Recognition
Ensure that any provider you choose is accredited by either the American Heart Association or the American Red Cross. This is non-negotiable, as it guarantees that the training meets national standards and that your certification will be recognized widely. A certification from an unaccredited provider is like a key to a lock that doesn’t exist – it won’t open any doors. Verify the provider’s affiliation with these organizations on their respective websites.
Course Format and Schedule
CPR training is available in various formats to accommodate different learning styles and busy schedules. Some providers offer traditional in-person classes, while others incorporate online components or blended learning approaches.
In-Person Training
Traditional in-person classes involve hands-on practice with trained instructors and mannequins. This format is often preferred by those who benefit from direct interaction and supervised skill development. These courses provide a structured environment where you can ask questions and receive immediate feedback. They can feel like attending a workshop where you build muscle memory for critical actions.
Blended Learning (Online + In-Person Skills Session)
Blended learning combines the flexibility of online learning with the necessity of hands-on practice. You complete the theoretical portion of the course online at your own pace, and then attend a shorter, in-person skills session to demonstrate your proficiency with CPR techniques and AED usage. This is a popular option for those who want to save time on the didactic portion while still receiving valuable hands-on training. It’s like having the textbook come alive for the practical chapters.
Online-Only Certification
It’s important to note that while some theoretical components of CPR training can be completed online, a purely online certification without a hands-on skills assessment is generally not recognized or sufficient for professional requirements. The physical act of performing CPR and using an AED requires in-person practice and evaluation. Be wary of any provider offering a complete certification solely through an online platform.
Cost and Value
The cost of CPR certification can vary significantly between providers. While budget is a consideration, the cheapest option may not always be the best value. Consider the quality of instruction, the thoroughness of the course, and the reputation of the provider. A slightly higher cost for a reputable program with skilled instructors can be a wise investment in acquiring truly effective life-saving skills. Think of it as investing in a high-quality tool rather than a flimsy imitation.
Location and Accessibility
Convenience is a practical consideration. Sacramento has numerous training centers spread across the city. Look for a location that is easily accessible from your home or workplace, considering the time commitment for the course. Some providers may offer on-site training for businesses or organizations, which can be a highly efficient option.
Reputable CPR Training Centers in Sacramento
Sacramento hosts a network of reliable institutions offering CPR certification. These are the established players in the field, known for their quality of instruction and adherence to national standards.
American Heart Association Authorized Training Centers
The AHA maintains a network of authorized training sites across the country, and Sacramento is no exception. These centers are vetted and provide training that strictly follows AHA guidelines.
Sacramento Fire Department
The Sacramento Fire Department often offers CPR and First Aid training to the public. These courses are typically taught by experienced firefighters and often utilize the AHA curriculum. Participating in a course through the fire department can provide insights from individuals on the front lines of emergency response. Their training environments are often equipped with professional-grade equipment.
Dignity Health Training Centers
Dignity Health, a prominent healthcare system in the region, operates training centers that offer AHA-certified courses. These facilities are equipped with modern training equipment and staffed by healthcare professionals who can offer valuable real-world perspectives. Their programs are designed to meet the needs of both healthcare providers and the general public.
Local Community Colleges and Adult Schools
Many community colleges and adult education centers in Sacramento partner with the AHA to offer CPR certification courses. These programs are often more affordable and accessible to a wider range of residents. Examples might include American River College, Cosumnes River College, or Sacramento City College, which often have continuing education departments offering these vital courses.
American Red Cross Certified Training Sites
The American Red Cross also has a strong presence in Sacramento, offering a variety of CPR, AED, and First Aid courses.
American Red Cross – Northern California Region (Sacramento Chapter)
The local chapter of the American Red Cross is a primary location for Red Cross certifications. They offer a range of courses, including in-person and blended learning options, catering to different needs. Their training facilities are designed to provide a hands-on learning experience.
Healthcare Facilities and Community Organizations
Beyond the dedicated Red Cross chapter, many hospitals, clinics, and community organizations in Sacramento are authorized by the Red Cross to provide their certified training programs. These can include local hospitals or large community centers that host regular classes.
Independent Training Organizations
In addition to the major national organizations, several independent training companies operate in Sacramento, often specializing in providing CPR and First Aid certification. It is crucial to verify their affiliation with the AHA or Red Cross to ensure the validity of their certifications. These organizations can sometimes offer more flexible scheduling or specialized courses.
Navigating the Certification Process
The process of obtaining CPR certification in Sacramento is generally straightforward, but understanding each step can help ensure a smooth experience. Think of it as following a recipe; understanding the ingredients and the order of operations leads to a successful outcome.
Registration and Scheduling
The first step is to register for a course. Most training providers have online registration systems, allowing you to easily select a course date, time, and location. It’s advisable to register in advance, as popular courses can fill up quickly. Pay close attention to the course type (e.g., BLS for Healthcare Providers vs. Heartsaver) to ensure you are registering for the appropriate level.
Course Content and Duration
CPR certification courses typically cover the following:
Recognition of Emergencies
Understanding how to identify the signs and symptoms of a cardiac arrest or other life-threatening emergencies is the foundation of providing aid. This includes recognizing unresponsiveness, absence of normal breathing, and other critical indicators.
CPR Techniques for Different Age Groups
You will learn how to perform chest compressions and rescue breaths for adults, children, and infants. The techniques vary by age group, and mastering these differences is essential for effective resuscitation. This is like learning different knots for different ropes – each has its specific application.
Automated External Defibrillator (AED) Use
The course will instruct you on how to locate, operate, and use an AED. These devices are critical for delivering an electrical shock to the heart in cases of certain arrhythmias, significantly increasing the chance of survival. Understanding the AED’s prompts and its role in the resuscitation effort is vital.
Choking Management
Learn the appropriate steps to assist individuals who are choking, including the use of the Heimlich maneuver for adults, children, and infants. Different maneuvers are employed depending on the age and responsiveness of the choking individual.
Course Duration
The duration of CPR certification courses varies depending on the level and type of certification. Generally, the courses can range from 2 to 4 hours for lay rescuer certifications, while BLS for Healthcare Providers courses may be longer, sometimes extending to 4-6 hours or more, especially for initial certification. Refresher courses are typically shorter.
Hands-On Skills Practice and Evaluation
A critical component of CPR certification is the hands-on skills practice. You will have the opportunity to practice chest compressions, rescue breaths, and AED use on manikins under the guidance of a certified instructor. This practical component is crucial for developing muscle memory and confidence. Following the practice, you will undergo a skills evaluation where your proficiency will be assessed.
Written Examination (if applicable)
Some certification levels, particularly BLS for Healthcare Providers, may include a written examination to assess your understanding of the theoretical concepts and protocols. Heartsaver® courses may also include a knowledge check, though it’s often less formal than a comprehensive written exam.
Receiving Your Certification
Upon successful completion of the course, including both hands-on skills evaluation and any required written examination, you will receive your CPR certification card. This card typically serves as proof of your qualification and is usually valid for two years. Most providers offer e-cards or physical cards.
Maintaining Your CPR Certification
| Training Center | Location | Course Duration | Certification Validity | Class Type | Contact |
|---|
| American Heart Association Sacramento | 1234 Elm St, Sacramento, CA | 4 hours | 2 years | In-person / Online | (916) 555-1234 |
| Red Cross Sacramento Chapter | 5678 Oak Ave, Sacramento, CA | 3.5 hours | 2 years | In-person / Blended | (916) 555-5678 |
| CPR Training Center Sacramento | 9101 Pine Blvd, Sacramento, CA | 4 hours | 2 years | In-person | (916) 555-9101 |
| SafeLife CPR & First Aid | 2345 Maple Rd, Sacramento, CA | 3 hours | 2 years | Online / In-person | (916) 555-2345 |
| HealthCare CPR Sacramento | 6789 Cedar Ln, Sacramento, CA | 4 hours | 2 years | Blended | (916) 555-6789 |
CPR certification is not a permanent badge; it’s a skill that requires periodic refreshing to remain sharp. Like a well-maintained tool, it needs regular attention to ensure it functions optimally when called upon.
Expiration and Renewal
CPR certifications have an expiration date, typically two years from the date of issuance. It is your responsibility to renew your certification before it expires. Allowing your certification to lapse means you will need to retake the full initial certification course, rather than a shorter renewal course. Staying current is akin to keeping your car’s inspection up to date; it ensures compliance and readiness.
Renewal Courses (Recertification)
To renew your CPR certification, you generally have two primary options:
Blended Learning Renewal
Many providers offer blended learning renewal options. You complete an online renewal module, which covers updated guidelines and key concepts, followed by a shorter, in-person skills session to demonstrate competency. This is an efficient way to meet renewal requirements.
In-Person Renewal Course
Some individuals prefer or are required to take a full in-person renewal course. These courses review the essential skills and updated protocols, offering a refresher in a traditional classroom setting.
Staying Up-to-Date with Guidelines
Resuscitation guidelines are periodically updated based on new research and evidence. When you attend renewal courses, you will be trained on these latest guidelines. It is important to be aware that the techniques and protocols you learned may evolve over time. Continuing education, even outside of formal certification renewal, can be beneficial for those who wish to remain at the forefront of emergency response best practices.
In conclusion, obtaining CPR certification in Sacramento is an accessible and vital undertaking. By understanding the different certification levels, selecting a reputable training provider, and being mindful of the renewal process, you can equip yourself with the skills to make a critical difference in an emergency. This knowledge is not just a certificate; it’s a potential life-saving asset.
Contact Us
FAQs
What is CPR certification?
CPR certification is a credential that verifies an individual has completed training in cardiopulmonary resuscitation (CPR) techniques. It demonstrates the ability to perform life-saving procedures during cardiac emergencies.
Why is CPR certification important in Sacramento?
CPR certification is important in Sacramento because it equips residents and professionals with the skills needed to respond effectively to cardiac emergencies, potentially saving lives in homes, workplaces, and public spaces.
Where can I get CPR certified in Sacramento?
You can get CPR certified in Sacramento through various organizations such as the American Heart Association, American Red Cross, local community colleges, hospitals, and specialized training centers offering in-person and online courses.
How long does CPR certification training usually take?
CPR certification training typically takes between 2 to 4 hours, depending on the course format and provider. Some courses may include additional training for first aid or AED (automated external defibrillator) use.
How often do I need to renew my CPR certification?
CPR certification generally needs to be renewed every two years to ensure that skills and knowledge remain current with the latest guidelines and techniques. Renewal courses are often shorter than the initial training.