
- Email: support@cprclassesnearme.com
Basic Life Support for Healthcare Providers
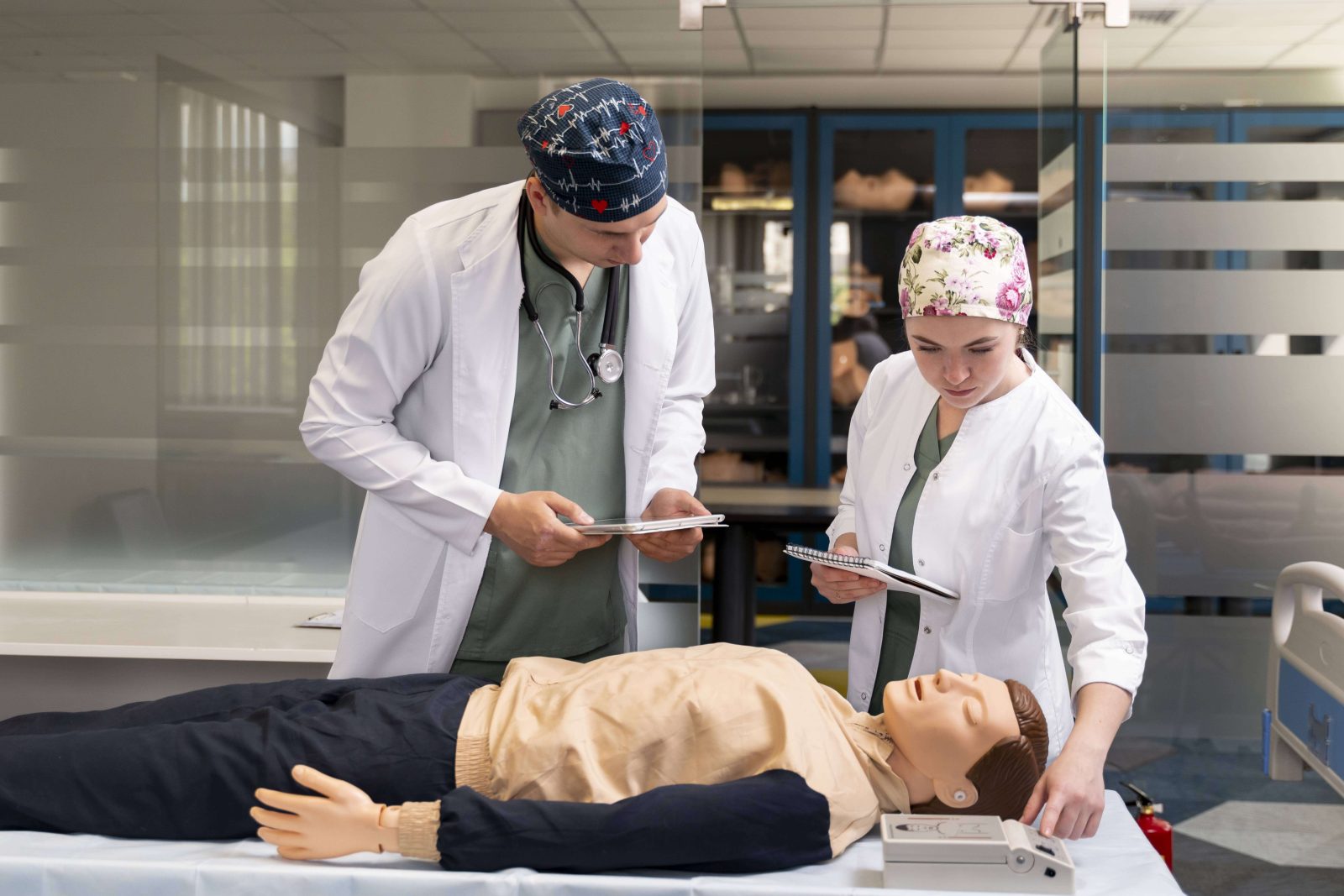
In the critical moments of a cardiac or respiratory emergency, healthcare providers are the first line of defense. Equipped with the knowledge and skills of Basic Life Support (BLS), they can intervene swiftly and effectively, potentially saving a patient’s life. This article dives deep into the core principles of BLS for healthcare providers, outlining the essential procedures and emphasizing best practices.
What is Basic Life Support for Healthcare Providers?
Basic Life Support (BLS) is a set of fundamental skills used to maintain minimal circulation and ventilation in an unresponsive patient until advanced care arrives. Designed for healthcare professionals and first responders, BLS training equips them to recognize life-threatening emergencies, perform high-quality cardiopulmonary resuscitation (CPR), and utilize an automated external defibrillator (AED) effectively.
BLS serves as the cornerstone of resuscitation efforts. By promptly initiating these interventions, healthcare providers can significantly improve a patient’s chances of survival during a cardiac arrest or respiratory failure.
Core Components of Basic Life Support for Healthcare Providers
BLS training for healthcare providers encompasses a comprehensive skill set focused on three key areas:
- Cardiopulmonary Assessment:
- Recognizing signs of unresponsiveness, absence of breathing, and abnormal pulse.
- Performing a systematic assessment using the CAB (Circulation, Airway, Breathing) approach to identify the nature of the emergency.
- High-Quality CPR:
- Delivering chest compressions at the appropriate rate and depth to maintain circulation of oxygenated blood throughout the body.
- Providing effective rescue breaths to ensure oxygen delivery to the lungs.
- Maintaining proper hand placement and body positioning for optimal CPR performance.
- Early Defibrillation:
- Recognizing the importance of early defibrillation in cases of cardiac arrest.
- Utilizing an AED effectively to analyze the patient’s heart rhythm and deliver an electrical shock if indicated, potentially restoring a normal heart rhythm.
Healthcare providers receive in-depth training on these core components, allowing them to perform BLS procedures with confidence and competence in a variety of healthcare settings.
Importance of Chain of Survival in BLS
The concept of the Chain of Survival underscores the critical interconnectedness of various steps in a successful resuscitation attempt. Each link in the chain represents a crucial action that, when performed effectively and promptly, significantly increases the likelihood of survival.
The Chain of Survival for BLS includes:
- Early Access: Bystanders calling emergency medical services (EMS) immediately.
- Early CPR: Healthcare providers initiating CPR as soon as possible.
- Early Defibrillation: Utilizing an AED to deliver a shock if indicated.
- Effective Advanced Care: Advanced medical interventions provided by EMS and hospital staff.
BLS training emphasizes the importance of each link in the Chain of Survival. Healthcare providers are trained to act swiftly and efficiently, ensuring a smooth transition to advanced care once EMS arrives.
Detailed Breakdown of BLS Procedures for Healthcare Providers
- Cardiopulmonary Assessment
The initial assessment in a BLS scenario involves a rapid evaluation of the patient’s responsiveness, breathing, and circulation. Healthcare providers follow the CAB (Circulation, Airway, Breathing) approach to determine the most critical intervention needed.
- Responsiveness: Gently tap or shake the patient’s shoulders while calling their name loudly. A lack of response indicates an unresponsive patient requiring immediate intervention.
- Airway: Open the airway using a head-tilt chin-lift maneuver if there is no suspected neck injury. Look, listen, and feel for signs of breathing. If the patient is not breathing or breathing inadequately, initiate rescue breaths.
- Breathing: Observe the patient’s chest for rise and fall. Listen and feel for the presence of air movement over the nose and mouth. If the patient is not breathing normally, begin rescue breaths.
- Circulation: Check for a carotid pulse in the neck for no more than 10 seconds. If a pulse is absent, initiate chest compressions.
- High-Quality CPR
Once an unresponsive patient is identified with absent breathing or abnormal pulse, CPR becomes the cornerstone of BLS intervention. Healthcare providers are trained to deliver high-quality CPR, which involves the following key elements:
- Chest Compressions:
- Locate the center of the chest, on the breastbone.
- Place the heel of the dominant hand over the center of the chest.
- Place the other hand on top of the first hand, interlocking fingers.
- Push hard and fast, at a rate of 100-120 compressions per minute.
- Allow for complete chest recoil after each compression.
- Minimize interruptions in chest compressions.
- Rescue Breaths:
- If the patient is not breathing normally, deliver rescue breaths.
- Pinch
- Rescue Breaths:
- Pinch the nose closed using your thumb and index finger.
- Create a seal with your mouth over the patient’s mouth.
- Deliver two breaths, each lasting one second.
- Observe chest rise with each breath.
- Ratio of Chest Compressions to Rescue Breaths:
- For single-rescuer CPR, the recommended ratio is 30 chest compressions to 2 rescue breaths.
- For two-rescuer CPR, the ratio is 15 chest compressions to 2 rescue breaths.
- Minimize Fatigue:
- CPR can be physically demanding. Providers are trained on techniques to minimize fatigue, such as proper body positioning and switching roles during CPR with another provider.
- Early Defibrillation
In the event of a cardiac arrest, early defibrillation is critical for restoring a normal heart rhythm. BLS training equips healthcare providers to utilize an AED effectively.
- AED Use:
- Turn on the AED and follow the clear voice prompts.
- Expose the patient’s chest and ensure no metal objects are touching their skin.
- Apply the AED pads as instructed by the device.
- The AED will analyze the heart rhythm and determine if a shock is necessary.
- If a shock is advised, ensure everyone is clear of the patient before the AED delivers the shock.
- Importance of Early Defibrillation:
- The chance of successful defibrillation decreases significantly with each passing minute. BLS training emphasizes the importance of using an AED as soon as possible after identifying a cardiac arrest.
Additional Considerations in BLS for Healthcare Providers
- Scene Safety:
- Healthcare providers are trained to assess the scene for any potential hazards before approaching the patient. This ensures their own safety and allows them to focus on patient care.
- Infection Control:
- Providers wear appropriate personal protective equipment (PPE) to minimize the risk of infection during resuscitation efforts.
- Communication and Documentation:
- Clear communication with EMS and other healthcare personnel is essential for a coordinated resuscitation effort.
- BLS training emphasizes the importance of accurate documentation of the assessment findings and interventions performed.
- Special Considerations for Infants and Children:
- BLS procedures for infants and children differ slightly from those for adults. Healthcare providers receive specific training on age-appropriate techniques for CPR and AED use.
- Continuous Learning and Skill Improvement:
- BLS skills need to be maintained through regular practice and refresher training. Healthcare providers are encouraged to participate in ongoing BLS training programs.
Conclusion
Basic Life Support (BLS) equips healthcare providers with the essential skills to intervene effectively in life-threatening emergencies. By mastering the core components of BLS – cardiopulmonary assessment, high-quality CPR, and early defibrillation – healthcare providers can significantly improve patient outcomes and potentially save lives. The emphasis on the Chain of Survival reinforces the importance of each step in the resuscitation process and the need for seamless collaboration between healthcare providers and EMS.
This article has provided a comprehensive overview of BLS for healthcare providers. If you are interested in becoming a BLS-certified healthcare provider, numerous organizations offer training programs that meet the current American Heart Association (AHA) guidelines. Remember, BLS skills are crucial for saving lives, and ongoing education and practice are essential for maintaining competence in these lifesaving techniques.
